Introduction:Splenic infarct (SI) is caused by thromboembolic events or other local or systemic factors leading to insufficient splenic blood supply. One of the most common causes of SI is an underlying malignancy, which has been associated with nontraumatic SI in up to a third of cases. The incidence, underlying etiology, optimal treatment, and prognostic relevance of SI in cancer patients (pts) are poorly characterized with data limited to a few, retrospective, single center case series.
Methods:We conducted a retrospective analysis of all radiologically-confirmed cases of SI in pts with any history of malignancy treated at Yale-New Haven Hospital during 2008-2017 to describe the incidence, treatment, and risk of recurrence of SI in cancer pts. Pediatric pts and cases of traumatic SI were excluded. Electronic medical records of eligible pts were reviewed and demographic, clinical, imaging and treatment characteristics as well as SI recurrence documented. Categorical and continuous variables among pts with and without recurrence of SI were compared using Pearson's χ2 test or Fisher's exact test and t-test with unequal variances, respectively. Multivariable logistic regression models that included variables associated with a higher risk of SI recurrence at a p-value of <0.2 in bivariate analysis were conducted to evaluate the impact of those variables on SI recurrence.
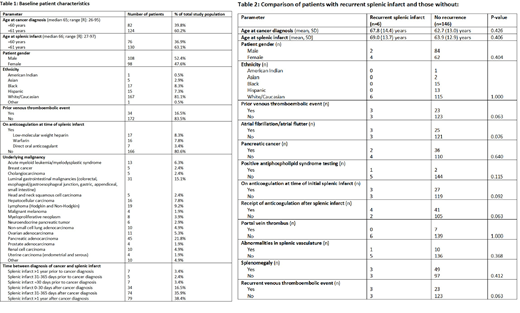
Results:206 pts were included in the analysis with baseline characteristics shown inTable 1.Thirty-four pts (16.5%) had a prior venous thromboembolic event (VTE), while 40 pts (19.5%) had been on anticoagulation (AC) for other indications at the time of SI. Diagnosis of SI was often made incidentally on CT or MRI during routine cancer surveillance (44.2%; n = 91) or initial cancer staging (5.8%; n = 12). Splenomegaly was present in 33% of cases (n = 68) with 90.8% of pts (n = 188) having an unremarkable splenic vasculature. Abnormalities in the splenic vasculature included splenic artery/vein thrombosis (2.9%; n = 6) or occlusion (1.5%; n = 3), external compression by local tumor (1.5%; n = 3), direct tumor invasion into the splenic vasculature (2.9%; n = 6), and portal vein thrombosis (4.9%; n = 10).
Following a diagnosis of SI, 22 pts (10.7%) were newly started on therapeutic AC and 36 pts (17.5%) continued on previously prescribed AC. Compared to those who were not anticoagulated, pts who were started or continued on AC after their diagnosis of SI were statistically more likely to have atrial fibrillation/flutter (29.3% vs. 12.2%; p = 0.003) or to have had a prior VTE (46.6% vs. 4.7%; p < 0.001). Pts newly started on AC following SI were more likely to have had a prior VTE (27.2% vs. 4.7%; p < 0.001) compared to pts who did not receive AC without a statistically significant difference in the rates of atrial fibrillation/flutter (22.7% vs. 12.2%; p = 0.186). Five of the 22 pts (22.7%) initiated on and five of the 36 pts (13.9%) continued on AC developed a subsequent VTE, respectively. There was no statistically significant difference in the risk of subsequent VTE among pts who continued or initiated AC compared to pts who did not receive AC (17.2% [10 out of 58 pts] vs. 12.8% [19 out of 148 pts]; p = 0.414).
Follow-up imaging was available for 152 of the 206 pts (73.8%). A recurrent or enlarging SI was detected in 6 pts (4.0%) at a median of 35 days following initial SI (range: 8-734 days). Anticoagulation was not associated with a reduction in the risk of subsequent SI. In bivariate analysis none of the baseline patient, treatment, or imaging characteristics were statistically significantly associated with a higher chance of SI recurrence, although prior and subsequent VTE (p = 0.063) and atrial fibrillation/flutter (p = 0.076) showed trends towards statistical significance (Table 2). In a multivariable logistic regression model, no variables were identified that were associated with a higher risk of SI recurrence.
Conclusion:In this large retrospective study of 206 cancer pts with SI, we showed that SI in this patient population are often an incidental finding with low risk of recurrence that is not impacted by AC. SI recurrence in cancer pts has a nonsignificant association with atrial fibrillation and prior VTE and therefore might arise as a cardioembolic event or as part of the underlying hypercoagulable state of malignancy. Additional prospective studies are needed to evaluate the risk and benefits of AC in this setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal